Pig-to-human kidney transplants. A blood test for Alzheimer’s. Birth control without a prescription. These were just a few of the advancements in health and medicine in 2024.

Link :
Young people don’t worry about their health the same way older individuals do. Of course, many Gen Zers and Millenials do prioritize their physical and mental wellbeing. But they are young, while the risk of life-changing conditions like heart disease, diabetes, chronic pain, and cancer increases with age. However, research shows that Gen Z and Millenials are not as safe as once thought. The number of cases of colon cancer has doubled in the United States since the 1990s. Especially in the age 20 to 49 demographic.
Colon cancer is also known as colorectal cancer, bowel cancer, or rectal cancer — depending on where the tumor begins. It’s also called the silent killer because there may be few or zero warning signs. And once the symptoms finally appear, the cancer has already progressed.
According to the Colon Cancer Coalition (CCC), colorectal cancer is the fourth most commonly diagnosed cancer, and the second leading cause of death due to cancer. Moreover, 30% of its diagnoses are for individuals under the age of 55. This has made it the leading cause of cancer death for men and the second leading for women under the age of 50.

The work-related death rate fell 95% in the U.S. between 1913 & 2015.
Labor union activism is often credited with the decline, but economic expansion is what made better working conditions possible in the first place.
Read more about this trend.
All economic activity involves some degree of physical risk. Credible data on work injuries and fatalities among our agrarian ancestors are difficult to come by. Yet agricultural work must have been quite unappealing, considering that so many people in the early 19th century preferred factory work over farm work.
Even today, notes the U.S. Department of Labor, agriculture “ranks among the most dangerous industries.” In 2011, the “fatality rate for agricultural workers was 7 times higher than the fatality rate for all workers in private industry; agricultural workers had a fatality rate of 24.9 deaths per 100,000, while the fatality rate for all workers was 3.5.” Likewise, the Workplace Safety and Health (WSH) Institute in Singapore found that global fatality rates per 100,000 employees in agriculture ranged from 7.8 deaths in high-income countries to 27.5 deaths in the Southeast Asia and Western Pacific regions in 2014. Manufacturing deaths ranged from 3.8 in high-income countries to 21.1 in Africa.

In this article, we examine airborne microplastics in greater detail, explore detection methods, consider what we currently know about their health risks and highlight various mitigation strategies.
Unpacking the origins of microplastics
Airborne microplastics are a growing concern due to their presence across diverse environments, from lively city centers to isolated, untouched corners of the world.

Researchers at the CUNY Graduate Center have made a groundbreaking discovery in Alzheimer’s disease research, identifying a critical link between cellular stress in the brain and disease progression.
Their study focuses on microglia, the brain’s immune cells, which play dual roles in either protecting or harming brain health. By targeting harmful microglia through specific pathways, this research opens new avenues for potentially reversing Alzheimer’s symptoms and providing hope for effective treatments.
Key cellular mechanism driving alzheimer’s disease identified.
Link :
Imagine your lungs, those essential organs responsible for getting oxygen into your blood, suddenly tasked with a new job: making blood itself. It sounds almost unbelievable, right? For centuries, we’ve been taught that bone marrow is the powerhouse of blood production. Yet, a groundbreaking discovery has just turned that conventional wisdom upside down.
Researchers at the University of California, San Francisco, have found that our lungs do far more than help us breathe—they’re also busy creating millions of platelets every hour, playing an unexpected and crucial role in our blood supply. This discovery not only challenges what we thought we knew about the body but also opens the door to new possibilities in understanding blood production and its implications for human health.
For centuries, the bone marrow has been recognized as the cornerstone of blood production. This soft, spongy tissue located within the cavities of our bones serves as a bustling factory for manufacturing the essential components of blood. It produces red blood cells, which carry oxygen to tissues; white blood cells, the immune system’s defenders against infections; and platelets, the fragments that form clots to prevent bleeding. These vital elements work together to sustain life, ensuring oxygen transport, immune defense, and wound repair. This process, called hematopoiesis, has been considered the exclusive domain of bone marrow, a belief deeply ingrained in medical science.

Racing closer to the Sun than ever before, the Parker Solar Probe is unlocking the secrets of our solar system’s fiery heart.
NASAs Parker Solar Probe has successfully transmitted a beacon signal back to Earth, confirming it is in good health and functioning normally after its record-breaking close approach to the Sun.
The mission operations team at Johns Hopkins Applied Physics Laboratory (APL) in Laurel, Maryland, received the signal just before midnight EST on December 26. During its closest approach on December 24, the spacecraft traveled at an astonishing 430,000 miles per hour and came within 3.8 million miles of the Sun’s surface, making it the closest any human-made object has ever been to our star.
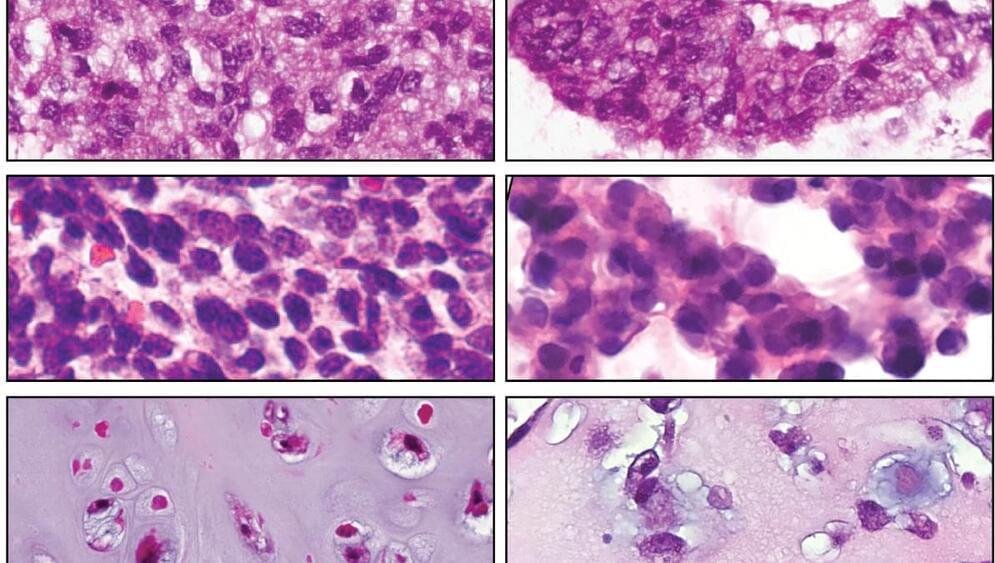
Investigators at the UCLA Health Jonsson Comprehensive Cancer Center have developed the largest collection of sarcoma patient-derived organoids to date that can help improve the understanding of the disease and better identify therapies that are most likely to work for each individual patient.
The approach, detailed in the journal Cell Stem Cell, uses patients’ own tumor cells that replicate the unique characteristics of a patient’s tumor allowing scientists to quickly screen a large number of drugs in order to identify personalized treatments that can target this rare and diverse group of cancers.
“Sarcoma is a rare and complex disease, which makes conducting clinical trials to identify effective treatments particularly challenging. Some of the rarer subtypes lack standard treatment altogether. Even when multiple therapy options are available, there is often no reliable, data-driven method to determine the best course of action for an individual patient. Choosing the most effective treatment is akin to searching for a needle in a haystack,” said Dr. Alice Soragni, the senior author of the study and assistant professor in the department of Orthopaedic Surgery at the David Geffen School of Medicine at UCLA. “Testing drugs with patient-derived tumor organoids has potential to help predict how a patient may respond to treatment, with the goal of improving patient outcomes for diseases where treatment options are often limited.”

Smartwatch bands from popular brands have been found to contain high concentrations of toxic for forever chemicals, also known as PFAS (per-and polyfluoroalkyl substances). These synthetic chemicals do not break down easily in the environment and build in our bodies over time, hence earning them the nickname of forever chemicals.
PFAS are used in various consumer products, including non-stick cookware, water-resistant clothes, carpets, mattresses, food wraps, and more. Exposure to PFAS has been linked to serious health problems, including increased risks of certain cancers, hormone disruption, weakened immune systems, and developmental delays in children. These chemicals can leach into water, soil, and food, making them a growing public health concern worldwide.
A new study published in the journal Environmental Science & Technology Letters has found that smartwatch bands made of fluoroelastomers contain a very high concentration of a forever chemical known as perfluorohexanoic acid (PFHxA).
