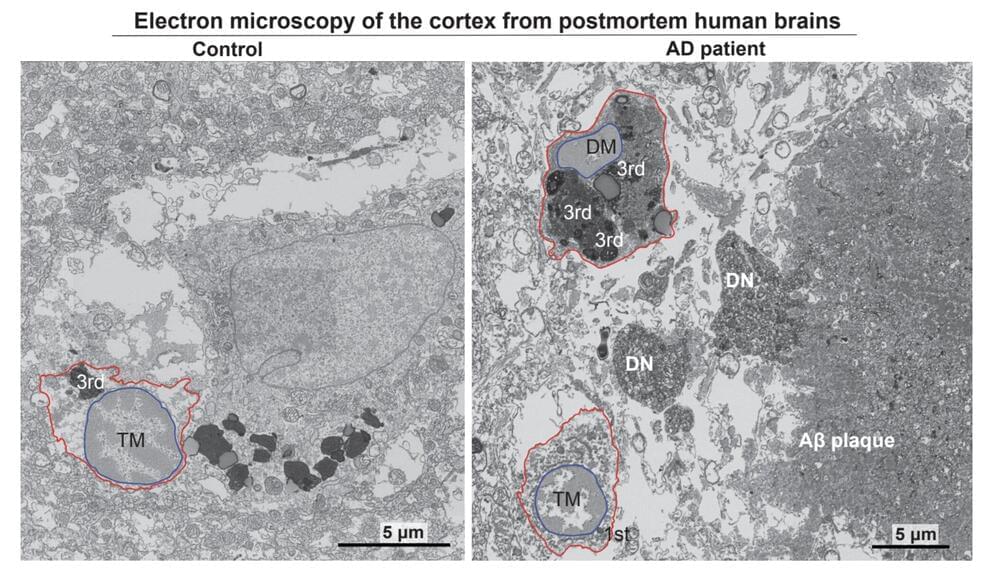
Researchers with the Advanced Science Research Center at the CUNY Graduate Center (CUNY ASRC) have unveiled a critical mechanism that links cellular stress in the brain to the progression of Alzheimer’s disease (AD).
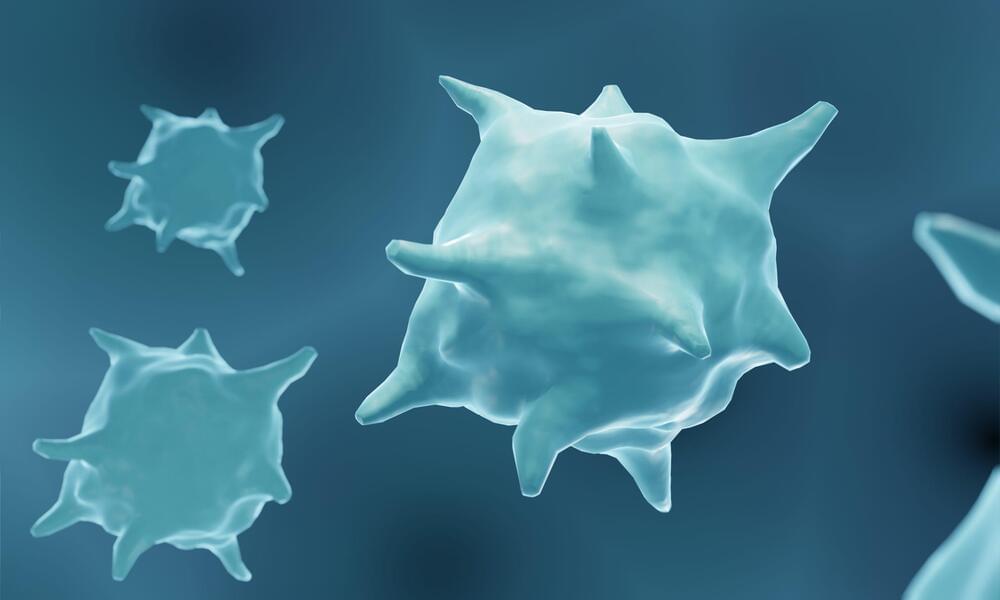
The study, published in the journal Neuron, highlights microglia, the brain’s primary immune cells, as central players in both the protective and harmful responses associated with the disease.
Microglia, often dubbed the brain’s first responders, are now recognized as a significant causal cell type in Alzheimer’s pathology. However, these cells play a double-edged role: some protect brain health, while others worsen neurodegeneration.